Meet the Speakers

PROF DON NUTBEAM
Sydney Health Partners / University of Sydney
Don Nutbeam is the Executive Director of Sydney Health Partners and a Professor of Public Health at the University of Sydney. Sydney Health Partners is an NHMRC-accredited Advanced Health and Research Translation Centre.
Don Nutbeam’s career has spanned senior leadership positions in universities, government, health services and international organisations including WHO and the World Bank. He was formerly Vice-Chancellor of the University of Southampton, UK, Provost of the University of Sydney, and Head of Public Health for the UK Government.
He is a public health scientist with research interests in the social and behavioural determinants of health, and in the development and evaluation of public health interventions. His current research focusses on the development and testing of interventions to improve health literacy in different populations.
Don is the current Chair of the Australian Health Research Alliance (AHRA).

A/PROF RACHEL SHELTON
Columbia University
Rachel Shelton, ScD, MPH is a social and behavioural scientist with training in cancer and social epidemiology, and expertise in implementation science, sustainability, health equity, and community-based participatory research. She is a tenured Associate Professor of Sociomedical Sciences at Columbia University’s Mailman School of Public Health, where she is Co-Director of the Community Engagement Core Resource at the Irving Institute for Clinical and Translational Research (CTSA) and Director of a university-wide Implementation Science Initiative.
Dr Shelton developed one of the first courses offered in implementation science in public health and has been an invited speaker and mentor for implementation science programs and trainings globally for the past ten years, including NIH’s Training Institute for Dissemination & Implementation Research in Cancer (TIDIRC), the Institute for Implementation Science Scholars, and implementation science training programs in Australia, Nigeria, Ireland, Mozambique, and Thailand. Additionally, she is a lead author in foundational textbooks in the field, including Dissemination and Implementation Research in Health and Practical Implementation Science, and has led national working groups and task forces on application of implementation science to promote health equity.
Dr Shelton has 15 years of experience conducting and leading mixed-methods, community-engaged research on advancing the science of implementation and sustainability of evidence-based interventions in community and clinical settings to address health inequities, particularly in the context of cancer prevention/control. Her research program is funded by numerous NIH institutions and foundations, including NIA, NCI, NIMHD, NCATs and American Cancer Society.

PROF LUKE WOLFENDEN
Columbia University
Prof Wolfenden is a behavioural and implementation scientist funded by an NHMRC Investigator grant. He is the Director of the National Centre of Implementation Science, Co-Director of WHO Collaborating Centre for NCD Program Implementation and Co-ordinating Editor of Cochrane Public Health. His research seeks to reduce the chronic disease burden in the community through undertaking policy-relevant evidence syntheses; trials of interventions to reduce modifiable chronic disease risks, and testing strategies to increase the adoption and implementation and scale-up of evidence-based interventions.

DR SANNE PETERS
University of Melbourne
Dr. Sanne Peters is a Postdoctoral Research Fellow in Implementation Science at the University of Melbourne.
She started her research career in Melbourne, at the Royal Children’s Hospital Education Institute in 2013. It was there that she was first able to pursue her interest in the health and education nexus. Sanne’s PhD research explored strategies aimed at improving knowledge translation in the training of general practitioners at the University of Leuven, in Belgium. During her postdoctoral work in Belgium and as Chair of the Implementation Working Group of the Guidelines International Network, Sanne has been facilitating bottom-up behaviour change processes that aim to increase the uptake of evidence-based clinical guidelines into practice.
At the University of Melbourne, Sanne works on multiple topics ranging from paediatric oncofertility to infection prevention and control in residential aged care facilities. Her work aims to address the barriers that slow or halt the uptake of proven health interventions and to identify the most effective ways to support improvements in healthcare practice to improve health outcomes.

A/PROF NATASHA HOWARD
South Australian Health and Medical Research Institute
A/Prof Natasha Howard is the Platform Lead: Implementation Science at the South Australian Health and Medical Research Institute (SAHMRI), Wardliparingga Aboriginal Health Equity Theme and Adjunct titleholder with Adelaide Medical School, The University of Adelaide.
Her program of work incorporates a systems view and privileges Indigenous knowledges to deliver mixed-method inter-disciplinary perspectives which aim to generate policy and practice-based evidence on the social determinants of health. Her experience spans both the health and social sciences, applying population approaches to investigate how the social and built environment enables and promotes cardiometabolic health and well-being, notably for priority populations.
A/Prof Howard, a non-Indigenous woman, is supporting and strengthening Aboriginal and Torres Strait Islander health researchers in her current leadership role. She has been active in advocacy and mentoring of the local population health community in both research and practice.

DR HELEN GOLDSMITH
Sydney Children’s Hospital Network
Dr Helen Goldsmith currently works in clinical research within the Sydney Children’s Hospital Network. She has been a registered nurse for over 25 years and has more than 20 years of experience conducting clinical trials, research projects and quality improvement initiatives with hospital clinicians, patients and carers in a variety of disciplines and settings.
Helen is a clinical research advocate, mentors clinicians in research, and uses behaviour change and implementation science strategies to embed research into clinical practice. She completed her PhD in 2018 investigating “The Incidence, Impact and Experience of Pain in Recently Discharged Adult Trauma Patients” at Sydney Nursing School, University of Sydney, where she is now a Research Affiliate. She also recently completed a Master of Health Leadership and Management at the University of New South Wales.

PROF JILL FRANCIS
University of Melbourne
Jill Francis, PhD, is Professor of Implementation Science at the School of Health Sciences, University of Melbourne (Australia), Implementation Lead for Health Services Research at the Peter MacCallum Cancer Care Centre (Australia), and Senior Scientist with the Centre for Implementation Research, Ottawa Hospital Research Institute (Canada); formerly Professor of Health Services Research at City University of London (UK) and Professor of Health Psychology at the University of Aberdeen (Scotland).
Jill is known for advancing theoretical and methodological developments in the field of implementation science in a wide range of clinical contexts. She has published over 200 peer-reviewed publications which have been cited over 29,000 times (Google Scholar).
Since arriving back in Australia in mid-2020, Jill has been a CI on funded projects to the value of around $30 million. She focuses largely on capacity building and supporting ECRs and MCRs, including leading the Implementation Research Group in Melbourne’s healthcare precinct and serving as a Co-founding Director of the HSR Fellowship program for the Melbourne Academic Centre for Health (MACH).

DR NICOLE NATHAN
University of Newcastle
Dr Nathan is an MRFF Investigator at the University of Newcastle who through her Fellowship is leading a program of research to identify how best to sustain the implementation of chronic disease prevention programs in community settings.
Dr Nathan is a health promotion research practitioner within Hunter New England Population Health (HNEPH) where for 20 years she has led the implementation and evaluation of Australia’s largest population-wide child obesity prevention service and research trials in community settings, in particular within schools (Good for Kids. Good for Life). During this time Dr Nathan has led the largest school-based implementation trials internationally. Such research has received national recognition, including awards from the Australian National Preventive Health Agency for research translation, and the NSW Government, and have yielded changes in NSW health, education and other non-government agencies’ policies and practices.
Dr Nathan’s research within the field of sustainability science will include the first trial internationally to test the effectiveness of strategies in sustaining school-based healthy eating and physical activity programs. As such it is being used to inform the research and practice of policy and practice locally, nationally and internationally.

DR JOANNA MOULLIN
Curtin University
Joanna C. Moullin, PhD, is a senior research fellow at Curtin University in Perth. She leads the Implementation Science Program in Curtin’s enAble Institute and is Deputy Director of the Research and Innovation Alliance between Curtin and WA Country Health Service. A pharmacist by profession, her research focuses on implementation of evidence-based interventions in a range of diverse settings.
Dr Moullin’s work in implementation science has centred on implementation frameworks, models and theories, implementation research methodologies, as well as pragmatic measure development. As part of her research, she has collated the core implementation concepts as the Generic Implementation Framework (GIF) and has worked extensively with the Exploration, Implementation, Preparation and Sustainment (EPIS) framework. Dr. Moullin is currently involved in various implementation studies and projects, for example: scaling-up Naloxone supply in the community and the implementation of means restriction for suicide prevention through the staged supply of medication.

A/PROF SERENE YOONG
Deakin University
A/Prof Yoong is a Heart Foundation Future Leader Fellow, Accredited Practising Dietitian and Associate Professor in Implementation Science at Deakin University with extensive experience in co-design, scale-up and evaluation of chronic disease prevention interventions in community settings including childcare centre and schools. She is also the Deputy Director of a NHMRC Centre for Research Excellence in Community-based Implementation science and Associate Director of the Centre for Nutrition and Preventive Health (GLOBE) at Deakin.
Serene has been involved in over 20 randomised controlled trials undertaken in community settings to improve implementation of evidence-based health promotion programs and has significant expertise in implementation science methods and training, publishing guidance on undertaking pilot and randomised controlled trials testing implementation innovations. Serene works closely with end-user agencies to ensure the impact and relevance of her work, leading to the successful scale-up of multiple innovations to improve child nutrition in childcare centres nationally and schools within NSW.

A/PROF DENISE O'CONNOR
Monash University
Denise O’Connor is Associate Professor and Co-Deputy Director of Musculoskeletal Health and Clinical Epidemiology in the School of Public Health and Preventive Medicine, Monash University. She is Director of the Australasian Satellite of Cochrane Collaboration Effective Practice and Organisation of Care, which publishes reviews of interventions to improve health care delivery and systems, and editor with Cochrane Musculoskeletal.
Denise is an implementation scientist and health services researcher and her research explores the causes of, and the design and evaluation of solutions to address, research translation problems. This includes reducing low-value care and improving uptake of effective and efficient models of healthcare service delivery. Denise is lead investigator of Wiser Healthcare, a national research collaboration that works in partnership with health agencies and consumers to ensure better value healthcare for Australians, with a particular focus on reducing overdiagnosis and overtreatment. A/Prof O’Connor has received over $20 million in competitive research funding and has over 100 publications.
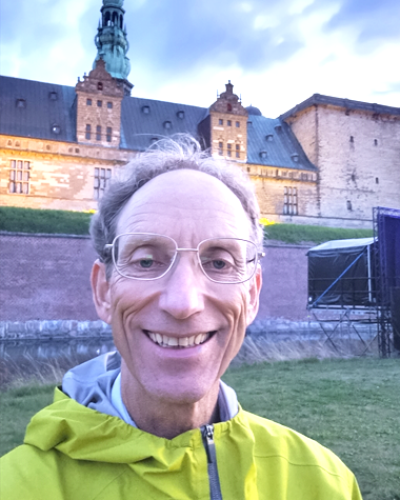
PROF ADRIAN BAUMAN
University of Sydney
Professor Emeritus Adrian Bauman AO was the Sesquicentenary Professor of Public Health and Director of the Prevention Research Collaboration at the University of Sydney until 2020. Prof Bauman is an internationally recognised public health physician, researcher and teacher. He has academic expertise in many aspects of the primary prevention of chronic disease, with an emphasis on physical activity and obesity prevention, including epidemiology, population-level interventions and policy research. He has a strong interest in research translation and in the evaluation of scaled-up programs and complex preventive health programs. Prof Bauman was appointed an Officer of the Order of Australia (AO) in 2021.

DR JACKIE YEOH
Central Adelaide Local Health Network
Dr Jackie Yeoh is a general practitioner currently working as the GP Integration Officer for Central Adelaide Local Health Network (CALHN) as well as a GP consultant in the Hospital Avoidance Supported Discharge Service run by the CALHN Integrated Care Directorate. She has been in the role of GPIO since late 2019, when it was set up as a collaboration between Adelaide Primary Health Network and CALHN, and works with two GP liaison nurses in the GP Integration Unit.
She has worked as a GP in the Adelaide region for 31 years, so brings a long experience of tackling problems from one side of the hospital wall to add to the last three years of learning how systems work on the other side and starting to bridge the gap between the two. From November 2021 to September 2022 she took on the position of medical lead for the CALHN COVID Care Centre and was involved in developing COVID pathways for the state, particularly in relation to the treatment of mild COVID with a view to preventing hospital admission and providing alternatives to ED attendance for people with COVID.
Jackie sits on the steering group of the Statewide Clinical Network for Chronic Pain and has enduring interests in chronic pain, mental health and the impact of both of these on general health and wellbeing.
She is committed to building better connections, communication and understanding between the different parts of the health system, so that all of those parts can work together for the benefit of those who use that system.

ECUSHLA LINEDALE
Health Translation SA
Ecushla Linedale is the Deputy CEO and Program Manager for Health Translation SA, South Australia’s NHMRC accredited Research Translation Centre. Ecushla is also the lead of Health Translation SA’s ‘Data-Driven Healthcare’ portfolio which aims to enhance the use of data-driven insights to improve health and healthcare in SA. She recently led the implementation of the Central Adelaide Local Health Network – PreHab Project. This project seeks to reduce the burden of post-operative complications, through the early and pro-active engagement with people referred for planned surgery using Personify Care’s digital health platform.
Ecushla has a PhD in Medicine and a breadth of experience spanning basic research, health services research and research translation. She is a titleholder and MBA candidate of the University of Adelaide, and previous member of the Australasian Institute of Digital Health – SA Branch Committee.
Her interest lies in connecting and supporting clinicians, researchers, consumers and industry to pragmatically use evidence to inform, develop and implement solutions to real world problems.

A/PROF NICOLE RANKIN
University of Melbourne
A/Prof Nicole Rankin is an Associate Professor in Evaluation & Implementation Science at the Melbourne School of Population and Global Health.
Nicole Ranking is an implementation scientist, whose research focuses on the science of research translation, including how evidence can be more rapidly translated into clinical practice, and how to improve patient and health service outcomes. A major focus of her research is lung cancer; her research portfolio in this context extends from screening, early detection, and management through multidisciplinary care through to palliation and survivorship.
Nicole’s interests extend to other cancers and psychosocial aspects of disease management. Her expertise is applied across a portfolio of research projects, teaching and mentoring clinician-researchers in implementation science methodologies and leading communities of practice.

DR LAUREN CHRISTIE
St Vincent's Health Network
Dr Lauren Christie is an occupational therapist clinician-researcher, clinical fellow of Australian Catholic University and the senior implementation science research fellow- allied health for St Vincent’s Health Network Sydney, where she leads the Allied Health Research Unit. She is also an affiliate of the Sydney Brain Centre, led by Professor Mark Parsons. Her PhD studies focused on clinician behaviour change in stroke and traumatic brain injury rehabilitation to support the delivery of constraint induced movement therapy (CIMT) programs using implementation science methods.
Lauren has been awarded over $900,000 in research funding, published in peer reviewed journals and presented her research internationally. In her role at St Vincent’s, she supports frontline allied health clinicians to engage in research. Her research program focuses on the implementation of effective interventions across the continuum of stroke recovery, upper limb rehabilitation and consumer decision making.

PROF NATASHA LANNIN
Monash University / Alfred Health
Professor Natasha Lannin is a Professor in the Department of Neurosciences at Monash University, Melbourne, where she leads the Brain Recovery and Rehabilitation Research Group and is the Chair of Occupational Therapy with Alfred Health. Professor Lannin specialises in scientifically rigorous clinical trials that inform the evidence-base of neurorehabilitation, and is best known for her whole-of-pipeline approach to improving clinical care, from phase 2 (pilot, feasibility trials) to phase 4 (implementation) trials. She holds a post-graduate certificate in Implementation Science from University of California San Francisco, and works alongside other trialists to plan for rapid translation of their trial findings into everyday clinical care in broader neurological populations (such as epilepsy) and rehabilitation groups (such as chronic respiratory conditions).

DR TAMINA LEVY
Flinders University
Dr Tamina Levy is a physiotherapist with over 30 years clinical experience in neurological rehabilitation. She works in the Advanced Practitioner Neurological Rehabilitation role at FMC-RAP and as a lecturer/researcher at Flinders University. Tamina completed her PhD in May 2021. In her PhD Tamina explored adherence to exercise in stroke survivors and has presented findings from her PhD at several conferences, including the World Physiotherapy Congress, 2021. Tamina’s area of research interest is around developing and implementing evidence-based rehabilitation programs for people with chronic neurological conditions, with a focus on behaviour change. She applies her knowledge across fields of clinical, teaching and research and supports allied health clinicians to engage in research.

PROF SANDY MIDDLETON
Maridulu Budyari Gumal (SPHERE)
Sandy Middleton is the Professor of Nursing, and Director of the Nursing Research Institute at St Vincent’s Health Network Sydney, St Vincent’s Hospital Melbourne and Australian Catholic University. She is a National Health and Medical Research Council (NHMRC) Leadership Fellow with an interest in stroke and implementation research and has obtained 106 grants totalling over $96.8 million.
Professor Middleton is Director of the Maridulu Budyari Gumal (Sydney Partnership for Health Education, Research and Enterprise – SPHERE) Implementation Science platform; and Director of the Maridulu Budyari Gumal (SPHERE) Nursing and Midwifery Implementation Science Academy. She is also Chair of the Steering Committee of the Australian Stroke Clinical Registry. Her program of stroke work was a finalist in the 2022 Engagement Australia Excellence Awards, for Outstanding Engagement for Research Impact.

PROF JEREMY GRIMSHAW
University of Ottawa
Dr Jeremy Grimshaw is an internationally recognized implementation scientist and evidence synthesist. He received a MBChB (MD equivalent) from the University of Edinburgh, UK. He trained as a family physician prior to undertaking a PhD in health services research at the University of Aberdeen. He moved to Canada in 2002. His research focuses on the evaluation of interventions to disseminate and implement evidence-based practice.
Dr Grimshaw is a Senior Scientist, Clinical Epidemiology Program, Ottawa Hospital Research Institute, a Full Professor in the Department of Medicine, University of Ottawa and held a Tier 1 Canada Research Chair in Health Knowledge Transfer and Uptake (2002 -2022). He is a Fellow of the Royal Society of Canada, the Canadian Academy of Health Sciences and a Corresponding Fellow of the Royal Society of Edinburgh. He has been awarded the CIHR Knowledge Translation award twice and the 2018 CIHR Barer-Flood career achievement award for Health Services and Policy Research. He has over 700 peer-reviewed publications.

ANNETTE RUHOTAS
Maridulu Budyari Gumal (SPHERE) Consumer
Annette is an active health consumer and community involvement representative at regional, state and national levels. Her interests include mental health, early childhood health, maternal health and health regulation. Her current health governance roles include: Medical Council of NSW, NSW Board of the Medical Board of Australia, Therapeutic Goods Administration, Advisory Council on Chemicals Scheduling, Sydney Partnership for Health, Education, Research & Enterprise (SPHERE), Maternal, Newborn & Women’s Clinical Academic Group, Schizophrenia Fellowship of NSW Limited (t/a One Door Mental Health) and Central & Eastern Sydney Primary Health Network, Clinical Council.
When not focused on elevating the views of health consumers, Annette is a company director and business consultant. As an unconventional Civil Engineer, she brings diverse experience from many sectors – Property, Construction, Sustainability, Environment, Social Services, Urban Planning and Health. She holds company director roles in private, government, social enterprise, not-for-profit and voluntary organisations. She is known as an astute critical thinker, respected for her collegiality and expertise in the Social elements of Environment, Social and Governance (ESG).
Annette holds tertiary qualifications in Bachelor Civil Engineering (Hons.); Bachelor Teaching – Secondary Science (Distinction); Certificate IV Remedial Massage.

JULIE GAWTHORNE
St Vincent’s Health Network
Julie is the Clinical Nurse Consultant in the Emergency Department at St Vincent’s Hospital, Sydney. She has a Masters in Nursing (Critical Care) and is enrolled in a PhD at Sydney University to study the implementation of nurse-initiated protocols in the Emergency Department.
Julie is a clinical researcher with experience in leading clinical practice and behaviour change to improve outcomes for patients presenting to emergency departments. Julie is passionate about promoting the role of clinician researchers and bridging the gap between academia and clinicians.

DR HOSSAI GUL
University of Technology Sydney
Hossai Gul is a transdisciplinary (TD) implementation scientist and practitioner, specialising in leading TD teams to implement evidence-based innovations into practice within complex systems. Hossai has worked within the Australian health and medical sector for over 10 years in health services, biomedical research, and health system and implementation science research.
Hossai has a Bachelor of Advanced Science, an Honours by thesis in cancer drug discovery, a Master of Research by thesis in bioinformatic analysis, and a PhD in Implementation Science and Complexity Science. Her current role is a lecturer and head of the Implementation Lab at TD School, University of Technology Sydney.

PROF BEN SMITH
University of Sydney
Professor Ben Smith is Deputy Director of the Prevention Research Collaboration in the Sydney School of Public Health and holds a conjoint appointment in public health with the Western Local Health District. His other affiliations include the Westmead Applied Research Centre and WHO Collaborating Centre in Physical Activity, Nutrition and Obesity.
The focus of his work is capacity building, evaluation and evidence translation to address chronic disease and health equity priorities.

DR JEAN-FRÉDÉRIC LEVESQUE
NSW Agency for Clinical Innovation
Dr Jean-Frédéric Levesque joined the NSW Agency for Clinical Innovation as Chief Executive in June 2017. He was previously Chief Executive of the Bureau of Health Information between 2013 and 2017. He brings to the ACI leadership in healthcare system analysis and improvement, combining experience in clinical practice in refugee health and tropical medicine, in clinical governance and in academic research. He is an Adjunct Professor at the Centre for Primary Health Care and Equity of the University of New South Wales.
Dr Levesque has a Medical Degree, a Masters in Community Health and a Doctorate in Public Health from the Université de Montréal, Canada. He is a Fellow of the Royal College of Physicians of Canada in Preventive Medicine and Public Health. He is a member of the Strategic Analytic Advisory Committee of the Canadian Institute of Health Information and a member of the HealthShare NSW Board.
Prior to joining NSW Health, he has held senior positions responsible for publicly reporting information about the Canadian health system at the Institut National de Santé Publique du Québec and the Commissaire a la santé et au bien-etre du Québec and was a Visiting Academic at the University of Melbourne.

JO MITCHELL
Australian Prevention Partnership Centre
Jo Mitchell is an independent consultant, senior advisor to ‘The Australian Prevention Partnership Centre’, a non-executive director of the Cancer Council NSW and has adjunct associate professor roles at the Universities of Sydney and NSW.
She was formerly a senior public sector executive and was the policy lead for population health in NSW. Her professional expertise is policy and the delivery of state-wide services and programs for health. She has significant experience in policy-relevant research, workforce development and purchasing and performance. Jo is passionate about prevention, equity and evidence informed strategy that drives health outcomes. She has degrees in science, nutrition and public health.

PROF BRENDAN McCORMACK
University of Sydney
Brendan’s research focuses on person-centredness with a particular focus on the development of person-centred cultures, practices and processes. He has engaged in this work at all levels from theory development to implementation science and through to instrument design, testing and evaluation. He is methodologically diverse but is most at home in participatory/action research. Whilst he has particular expertise in gerontology and dementia practices, his work has spanned all specialities and is multi-professional. Visit www.cpcpr.org for further info.
Brendan also has a particular focus on the use of arts and creativity in healthcare research and development. He has more than 600 published outputs, including 240 peer-reviewed publications in international journals and 12 books. He was the founding editor of the “International Journal of Older People Nursing” and is currently ‘Editor Emeritus’ of the journal. Brendan is a Fellow of The European Academy of Nursing Science, Fellow of the Royal College of Nursing, Fellow of the Royal College of Surgeons in Ireland and Fellow of the American Academy of Nursing.
In 2014 he was awarded the ‘International Nurse Researcher Hall of Fame’ by Sigma Theta Tau International and listed in the Thomson Reuters 3000 most influential researchers globally. In 2015 he was recognized as an ‘Inspirational Nursing Leader’ by Nursing Times (UK nursing magazine) and in 2019 was listed in the New Year ‘Top 100 outstanding nurses’ by the Twitter Group #wenurses. Most recently, Brendan was featured in the Wiley Publishers ‘Inspiring Minds’ short films series. In 2022 Brendan was selected as a member of The Academia Europaea.

A/PROF MICHELLE BARAKAT-JOHNSON
Sydney Local Health District
Michelle is the Skin Integrity Lead for Sydney Local Health District (SLHD), an Associate Professor at the Faculty of Medicine and Health, University of Sydney and a Research Fellow at the University of Huddersfield, UK.
Michelle’s expertise is in skin integrity, implementation science and pressure injury prevention. In 2015, she led a translational practice change project across SLHD which resulted in a reduction in pressure injury incidence (51.4%) and prevalence (71.4%) and a $4 million reduction in health care costs over a 5-year period. The project was recognised locally and nationally through awards, presentations and publications.
Michelle is the lead investigator of several funded translational studies and has achieved $8 million in research funding since completing her PhD in 2019. Michelle was recently awarded the Research Action Sax Institute Award and the Rita and Cornforth Medal for Research Excellence 2020 at the University of Sydney.

DR MITCHELL SARKIES
Sydney Health Partners / University of Sydney
Dr Mitchell Sarkies is a Senior Lecturer and NHMRC Emerging Leadership Fellow at the Sydney School of Health Sciences. Dr Sarkies leads the Innovation and Methods Stream for the Sydney Health Partners Implementation Science Program and is a member of the Academic Implementation Science Network, which supports advancements in the science of implementation in health.
Dr Sarkies is a health services researcher and implementation scientist with a clinical background in physiotherapy. Dr Sarkies leads multiple programs of research harnessing implementation science and complexity science to enhance evidence-informed models of care of hip fracture; developing an implementation strategy for improving the detection of familial hypercholesterolaemia; implementing a primary-tertiary shared care model for scaling up genetic medicine; and implementation of evidence and consensus-based perioperative care pathways to reduce unwarranted clinical variation in elective surgery.